From the preparation and discomfort, to the recovery and outcome, find out what it’s like to have an ECV for a breech baby in pregnancy.
If you’ve been following any of my pregnancy updates, you’ll have learned that after a very easy seven months, we hit a few minor blips towards the end of the final trimester!
At 34 weeks, the fetal growth was tracking low (5th centile). Finding this out caused a lot of anxiety, especially when we were told it might be recommended to have a c-section at 37 weeks. By 36 weeks, he’d grown a good chunk, so we were allowed to wait and see what happened.

The other issue was that he was sitting in a breech position with his legs up (extended breech). He seemed determined to stay up in his cosy spot, with his giant head rubbing against my ribcage! He’d been there a while too – well over a month, maybe longer. It’s unusual for a baby not to have turned head-down this point. In fact, only around 4% are still in the breech position by week 37.
After consultations with the breech team at the hospital during week 36, we came up with a plan. Firstly, I’d spend the week trying everything in my power to turn him naturally.

I booked appointments with an acupuncturist and chiropractor, as well as practising the various inversions recommended on the Spinning Babies website. You should have seen me – I spent a lot of time hanging upside-down off the sofa!

We even bought Moxa sticks and tried moxibustion. I’d never heard of this before, but it’s a Chinese medicine technique with a high success rate, where you burn a mugwort stick and hold it close to an acupuncture energy line point on your little toes. I put in a lot of hours to trying to shift the baby naturally!

We decided that if the baby hadn’t flipped by the end of week 37, we’d go ahead with an appointment at the hospital for an external cephalic version (ECV).
Having an ECV for a breech baby: My real-life story
What is an external cephalic version (ECV)?
I had never heard of this procedure before 30+ weeks of pregnancy, but I quickly swotted up! This procedure is always carried out in hospital, just in case there are any complications.
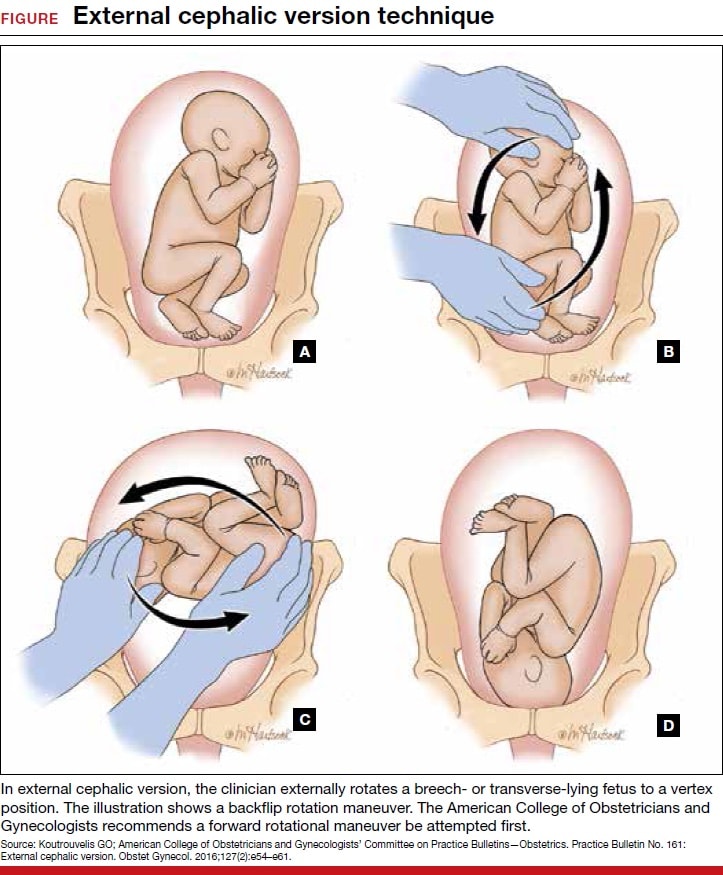
It’s where a consultant uses their hands on the outside of the tummy and attempts to manoeuvre the baby from its breech position, to place its head down towards the pelvis. It’s only attempted after the baby has been monitored and scanned to check conditions are suitable.
What happens before an external cephalic version (ECV)?
Despite my best efforts, our little boy was still breech by the day the ECV was booked for. We arrived at the hospital around 2pm and waited a little while in triage.
After around thirty minutes I was collected by a lovely midwife named Clare, and we were shown to a room in the labour area of the hospital. There was something quite exciting about snooping around the hospital we’d be returning to soon to have the baby! We met a few of the people who work there, spent time in a room used for labour and even heard a few (mildly terrifying) sounds of someone giving birth. All good preparation!

I changed into a hospital gown, got comfortable on the bed, and then was hooked up to the CTG monitor for around 15 minutes. This machine tracks the baby’s heart rate. I also had my blood pressure and oxygen levels checked.

Around half an hour passed and the midwife returned with one of the doctors who would be helping with the procedure. I was given an injection of Terbutaline into my thigh – a drug that helps to relax the uterus. I had been warned that it might make me feel like my heart was racing – just what I needed when I was anxious!
It was quite stingy, and made my muscle spasm. I sipped on water and took some deep breaths. I also played some soothing music to try to stay relaxed. I was happy to put my new hypnobirthing techniques to use.
The drug took around 15 minutes to work. During this time the midwife also got me set up with some gas and air (Entonox) which I could suck on during the procedure if I needed it.

Gradually, the room started to fill up with people who would be involved in the ECV procedure. A 5th year student popped her head around the door and asked if she could watch. Then, another midwife arrived and said ‘I’ve never seen an ECV – would it be ok to come and watch?’ Then, we had the doctor, our midwife Clare, and shortly after the consultant turned up too. It was a full house! I said yes to everyone, although with hindsight, I think I wish I’d passed on the extra spectators!
An ultrasound screen was wheeled in, and everyone settled in ready for the procedure to begin.
What happens during an external cephalic version and is it painful to have an ECV?
The one big thing I’d say about an ECV is that it’s quick! I’d heard they could be uncomfortable and painful, but I’d decided I was willing to go through it as the options of breech delivery (either vaginally or via c-section) were sounding complicated and had several added risks.
So, what did I experience? The doctor lowered the bed right back so that my back was flat, giving her a flat surface to work from. There was a quick scan using ultrasound to see the baby’s exact position, and then a discussion to decide whether it’d be easier to try to rotate him clockwise or anti-clockwise. The key was giving him the shortest, easiest route!
Then, the ECV procedure began. The doctor placed her hands on the edges of my abdomen and started to move the baby around so that his head was no longer by my ribs. This first attempt took around a minute and a half.
I’d describe the feeling as uncomfortable and unnatural, but it wasn’t seriously painful. It was more of a wrenching feeling, like someone was really grabbing at my tummy and twisting it, rather than the sort of pain you get when you cut yourself or hit something! It never made me yelp out in pain or ask them to stop.
One thing that was difficult was that after eight months of protecting my baby bump, it felt quite traumatic to have someone trying to intervene like this. That got to me a bit!
Unfortunately, this first attempt was unsuccessful. Then, the consultant who had more experience performing ECVs swiftly stepped in for attempt two. He tried a slightly more meticulous approach, reaching deeper into my pelvis area for where the bum and feet were, hoisting them upwards towards my tummy button, and then starting to rotate the baby around. He was gripping hard and I could feel a lot of pressure across my tummy area.
I sucked on some gas and air, and practised some breathing exercises with my partner. I got quite weepy towards the end of the second attempt. I remember the feeling of my lip quivering and quivering as tears pricked into the corners of my eyes. I don’t know if it was the headrush from the Entonox, the Terbutaline giving me palpitations, the emotion of the ordeal in general or just having so many people watching! I felt pretty overwhelmed, but it wasn’t pain causing the tears.
I didn’t watch much of what was going on. I chose to look into Macca’s eyes for comfort, while listening to words of encouragement from everyone in the room.
The second attempt took just over three minutes…
And then the magic words: “he’s rotated!”
Success!
The consultant reached for the ultrasound and showed everyone in the room the baby’s new position. There he was with his head down in my pelvis and his bum up towards my ribs!
The emotion washed over me at this moment too! With only a 40% chance of it working, I couldn’t quite believe it! I felt a bit shell-shocked, like I wasn’t totally present in my body. To be honest, it was a day or so before it all really sank in!

What happens after an ECV (external cephalic version)?
The room cleared quickly after the procedure was complete. I remained on the bed and was hooked up for more CTG monitoring to check the baby had coped ok with the ECV. He seemed very happy still. His heart rate was strong and I started to feel his kicks and movements in different parts to before!
After 15-20 minutes of monitoring, the midwife said I could get ready to go home. I was quite jittery and shaky (common side effects of the drug, but perhaps also the adrenaline come down) so I dressed slowly. I was also feeling pains similar to period pains, so the midwife brought me some paracetamol. After being at the hospital for just under three hours, we headed home.
How do you recover from an external cephalic version (ECV)?
I’m sure everyone reacts differently, but for me, I felt pretty exhausted for the rest of that day. I took it very easy that evening, used a heat pack to help with the pain and kept some paracetamol by the bed in case the pain was bad during the night. I woke up around 2am with the same feelings similar to period pains,
I didn’t sleep a lot more, but with the combination of being 37 weeks pregnant and my intermittent pregnancy insomnia, it’s not totally surprising. The next day I eased into the day with a relaxing bath. I felt a bit bruised. I even had a couple of marks on each side of my tummy, which looked like where the skin had been dragged. They’ve since gone down though.

What to check for after an ECV (external cephalic version)?
The midwife left me with a few things to keep an eye on after my ECV. The principal one was to go straight in if I noticed any change in the baby’s movements. I was also told to report any bleeding and to be on the watch for early signs of labour. Thankfully, it’s been smooth sailing since!
Why did I choose to have an ECV?
Finding out that your pregnancy has any complications is stressful. Everyone hopes for an easy route through, but it’s rare to make it to the finish line without some additional worries.
While in the UK it’s possible to have a breech baby vaginally, it comes with a lot more risk than a standard cephalic (head down) birth. Our hospital said we’d need to be referred to a different hospital where they had specialist midwifes who had more experience with these kinds of births. There were also more risks associated with a breech labour, such as cord prolapse or the head getting stuck.
If he was still breech then the other option was to have a caesarean section. This isn’t something I’d actively choose unless it was the best option for the baby. I have a few reasons for feeling this way. Most women recover from a vaginal birth more quickly. I’ve also felt like I’d like to experience what labour feels like.
Nine months ago, I probably would have suggested I’d want all the pain relief or a c-section, but being on this crazy journey has made me want to experience every element, including a vaginal birth. I know it’s beyond my control though, so we’ll see what happens when we get to that!

What are the pros and cons of an ECV?
There are a few things I thought about when deciding whether to go ahead with the ECV.
Pros
- Increased chance of vaginal delivery
- Removes risks associated with breech deliveries (cord prolapse, head stuck, trauma to baby’s bones)
- Reduced risk of needing a caesarean section
Cons
- 0.5% chance of distress to baby during the procedure which could require immediate c-section
- Uncomfortable for mum
- Small risk of bleeding or damage to womb
- Chance it could be unsuccessful
- Even if successful, there’s a 5% chance the baby could turn back to the breech position before labour

My overall thoughts on the ECV procedure
Now it’s done and I’ve had a few days to recover, I’m so relieved I went through with it! We’d been weighing up our options for breech births (vaginally or c-section) and both were feeling like they had their risks. To now have our baby sitting in the best position for a safer labour means a lot!
There’s no denying that the ECV was uncomfortable, but for three hours in hospital and a day taking it easy, it’s a small price to pay to give our little boy a better start in life (hopefully!)
If at our next scan we find out that he’s flipped back, there’s no denying I’d be very disappointed. However, I’d be tempted to opt for another ECV if it’d help. It wasn’t so bad I couldn’t face going through it again!
I hope reading my real-life story helps you if you’re going through a similar situation. I found very few personal stories that gave details about what the process was like and what to expect before and after. I also read a lot of scaremongering stories that dwelled on the risks and complications. When you dive into the stats, you’ll discover that complications are very unlikely with an ECV.
I’m not here to advise you on any medical situations as everyone is different, but hopefully reading this post will help you decide whether to try an ECV or not. If you have any questions, feel free to leave them in the comments or drop me an email!
If you’d like to read about my pregnancy journey, take a look at these posts:



Thank you so much for your encouraging story. I am 36 weeks pregnant and breech. My goal has always been for a natural birth but family and friends have discouraged a version. Thank you for giving me hope.
Thanks Sarah! I’m so glad you read this post and I have everything crossed for you. It’s not the situation any of us wanted to be in – but it can definitely still work out! Sending positive vibes for your little one to turn! Cx